The diagnosis of a brain tumor is always a shock for those affected and is associated with great anxiety and a cut in the normal rhythm of life. In this situation, it is important to find suitable doctors who have the expertise to treat the tumor properly and whom patients can trust.
Brain tumors may occur in all age groups and very often show a complex clinical picture. The minimally invasive and microsurgical treatment of brain tumors is one of Prof. Feigl’s main focuses. His patients receive extensive medical, nursing, psycho-oncological (relating to mental effects) and physiotherapeutic care throughout the entire treatment process and beyond. The treatment is coordinated by the Hirntumorzentrum Bamberg (brain tumor center), which Prof. Feigl founded in 2013.

Individual Therapy Planning and Aftercare at Hirntumorzentrum Bamberg
All of Prof. Feigl’s patients who undergo surgery for a brain or spinal tumor
(= in the area of the spine) are regularly followed up as part of the interdisciplinary consultation hours of the Brain Tumor Center.
In order to achieve an optimal treatment result, Prof. Feigl always draws up an individual therapy plan, using all currently available diagnostic and therapeutic methods according to the latest scientific standards. According to Prof. Feigl, the basic principle applies: The patient as a human being is always the center of all treatment decisions.

Therapy Options
In cases of brain tumors, an individual treatment plan is drawn up for each patient in the weekly Neurooncological Tumor Conference. In the field of radiotherapy and radiooncology (includes medical and physical procedures to support radiotherapy), we can offer our patients radiosurgical treatment in addition to Intensity-Modulated Radiation Therapy (IMRT) and tomotherapy, if required.
The irradiation technique IMRT enables a homogeneous dose distribution within the tumour by precisely adapting the radiation to the tissue. This allows a higher or lower dose of radiation to be absorbed depending on the density of the body part. This guarantees that surrounding structures are spared and enables targeted radiation of specific areas of the tumor.
The radiosurgical treatment (= radiation therapy with a very high dose in a single session) is carried out in collaboration with our cooperating partners, if required. All treatment plans developed in the clinic follow recognized guidelines and treatment recommendations based on the results of international scientific studies.
Brain Tumors and Awake Surgeries

Brain tumors arise from degenerated supporting cells of the brain (= cells that support the tissue) and therefore grow infiltratively (= into neighboring brain structures). A distinction is made between low-grade (benign) WHO I° and II° and higher-grade (malignant) WHO III° and IV°.
Brain tumors can cause a variety of symptoms. When brain tumors grow in the area of speech centers (Broca’s and Wernicke’s) and in the connecting pathways (e.g. fasciculus arcuatus), patients experience speech or word-finding disorders.
Other symptoms, depending on the location and size of the tumor, range from signs of intracranial pressure with headaches, nausea and vomiting to seizures. If the brain tumor is located in the area of the motor center (= involving movement), it can cause sensory disturbances and even paralysis.
In cases of brain tumors, a detailed clinical neurological examination with neuroradiological imaging in the MRI (“tube”) must be performed. In addition, a thin-slice CT of the skull or spine in the area of the tumor may be required to assess the bony structures.
As a first step, a detailed neurological and neuroradiological diagnosis is performed. Thin-slice MRI images (1 mm or less layer thickness) with contrast medium, native, T2 and CISS special sequences are required for imaging with different highlighting. This allows visualization of nerves and brain circuits (using tractography) and specific areas of brain function (using a functional MRI).
If necessary, a special examination, navigated transcranial magnetic stimulation (nTMS), is also performed. With this method, those areas of brain function that have been displaced by a tumor are visualized even more precisely than with a functional MRI. These data are needed for 3D
(= three-dimensional) and VR (= virtual reality) imaging in terms of surgical planning, patient education and intraoperative neuronavigation (“GPS for the brain”).
With many low-grade brain tumors, treatment is completed after a full resection. However, for higher-grade or malignant tumors, follow-up treatment must always be carried out, consisting of either chemotherapy, radiotherapy or combined radiochemotherapy. For this purpose, an individual treatment plan is always provided for the patient on an interdisciplinary basis.
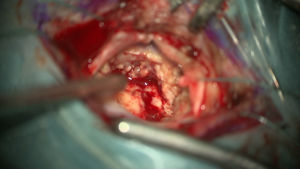
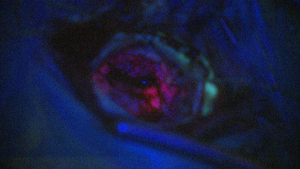
After a detailed neurological and neuropsychological examination, surgery in the awake state is performed for tumors in the area of the speech center, if possible. Only awake surgery allows permanent monitoring of speech function during tumor removal, thus ensuring the best possible tumor removal and minimal risk of loss of speech function. For better visualization, Prof. Feigl always uses 5-ALA fluorescence for higher-grade brain tumors (Figures 1 and 2: The first image shows the brain surface under the microscope with white light, the second with blue light. Under blue light, the tumor fluoresces
(= glows) and can be clearly distinguished from healthy brain tissue during removal).
Continuous awake craniotomy (CAC), co-developed by Prof. Feigl, is used for these awake surgeries. This method allows surgeons to operate on the patient with pain medication only, rather than subjecting them to general anesthesia. Patients are monitored during surgery by a neuropsychologist who continuously tests their speech function. Using direct brain stimulation (brain mapping), the brain function areas can be precisely localized during tumor removal and thus protected.
Brain tumors arise from degenerated supporting cells of the brain (= cells that support the tissue) and therefore grow infiltratively (= into neighboring brain structures). A distinction is made between low-grade (benign) WHO I° and II° and higher-grade (malignant) WHO III° and IV°.
Brain tumors can cause a variety of symptoms. When brain tumors grow in the area of speech centers (Broca’s and Wernicke’s) and in the connecting pathways (e.g. fasciculus arcuatus), patients experience speech or word-finding disorders.
Other symptoms, depending on the location and size of the tumor, range from signs of intracranial pressure with headaches, nausea and vomiting to seizures. If the brain tumor is located in the area of the motor center (= involving movement), it can cause sensory disturbances and even paralysis.
In cases of brain tumors, a detailed clinical neurological examination with neuroradiological imaging in the MRI (“tube”) must be performed. In addition, a thin-slice CT of the skull or spine in the area of the tumor may be required to assess the bony structures.
As a first step, a detailed neurological and neuroradiological diagnosis is performed. Thin-slice MRI images (1 mm or less layer thickness) with contrast medium, native, T2 and CISS special sequences are required for imaging with different highlighting. This allows visualization of nerves and brain circuits (using tractography) and specific areas of brain function (using a functional MRI).
If necessary, a special examination, navigated transcranial magnetic stimulation (nTMS), is also performed. With this method, those areas of brain function that have been displaced by a tumor are visualized even more precisely than with a functional MRI. These data are needed for 3D (= three-dimensional) and VR (= virtual reality) imaging in terms of surgical planning, patient education and intraoperative neuronavigation (“GPS for the brain”).
With many low-grade brain tumors, treatment is completed after a full resection. However, for higher-grade or malignant tumors, follow-up treatment must always be carried out, consisting of either chemotherapy, radiotherapy or combined radiochemotherapy. For this purpose, an individual treatment plan is always provided for the patient on an interdisciplinary basis.
After a detailed neurological and neuropsychological examination, surgery in the awake state is performed for tumors in the area of the speech center, if possible. Only awake surgery allows permanent monitoring of speech function during tumor removal, thus ensuring the best possible tumor removal and minimal risk of loss of speech function. For better visualization, Prof. Feigl always uses 5-ALA fluorescence for higher-grade brain tumors (Figures 1 and 2: The first image shows the brain surface under the microscope with white light, the second with blue light. Under blue light, the tumor fluoresces
(= glows) and can be clearly distinguished from healthy brain tissue during removal).
Continuous awake craniotomy (CAC), co-developed by Prof. Feigl, is used for these awake surgeries. This method allows surgeons to operate on the patient with pain medication only, rather than subjecting them to general anesthesia. Patients are monitored during surgery by a neuropsychologist who continuously tests their speech function. Using direct brain stimulation (brain mapping), the brain function areas can be precisely localized during tumor removal and thus protected.
Figure 1 and 2:
OP Images in Comparison
Figure 1 and 2: OP Images in Comparison